


 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 19-2-2016
Date: 2025-02-05
Date: 2025-02-05
|
Definition
• A malignant epithelial tumour arising in the colon or rectum.
* Note that only tumours that have penetrated through the muscularis mucosae into the submucosa are considered malignant at this site. this contrasts with carcinomas at other sites where a breach of the basement mem brane directly underlying the epithelium is sufficient for the categorization of an epithelial tumour as malignant.
Epidemiology
• third most common cancer in the UK, with a lifetime risk of 1 in 16 men and 1 in 20 women.
• Second most common cause of cancer- related deaths.
Aetiology
• A diet high in animal fat and low in fibre, together with a sedentary lifestyle, increases the risk.
• Other associations include idiopathic inflammatory bowel disease, FAP, and hereditary non- polyposis colorectal cancer (HNPCC).
Carcinogenesis
• Most develop through a sequence of aberrant crypt focus (dysplasia in a single crypt) → adenomatous polyp → invasive carcinoma.
• Common genetic aberrations include the loss of APC, TP53, and SMAD4.
• Some tumours are characterized by the inactivation of mismatch repair genes, recognized by the epiphenomenon of microsatellite instability.
Presentation
• Change in bowel habit, tenesmus, abdominal pain, iron deficiency anaemia.
• Asymptomatic tumours may be discovered via screening or surveillance programmes.
Macroscopy
• Most tumours grow as polypoid masses projecting into the bowel lumen, often with areas of surface ulceration (fig. 1). Some tumours, particularly in the distal colon, form circumferential stenosing lesions.
• the cut surface shows a firm, white tumour mass in the bowel wall.
• Large pools of gelatinous material are seen in mucinous carcinomas.
Histopathology
• the vast majority are adenocarcinomas, i.e. infiltrating malignant epithelial tumours showing evidence of glandular differentiation.
• Well- differentiated tumours show plentiful tubular formation, whereas poorly differentiated tumours show minimal gland formation.
• Most tumours are well/ moderately differentiated and often contain abundant necroinflammatory debris within the glandular spaces (so- called ‘dirty’ necrosis).
• ~10% of colonic and 30% of rectal tumours show extensive mucin production, such that the malignant cells are seen floating in large pools of extracellular mucin; these are termed mucinous adenocarcinomas.
• Patients with tumours which have a pushing margin and/ or associated with a marked increase in tumoural lymphocytes have a better prognosis.
• tumour regression, with fibrosis, is assessed using the Mandard Grade.
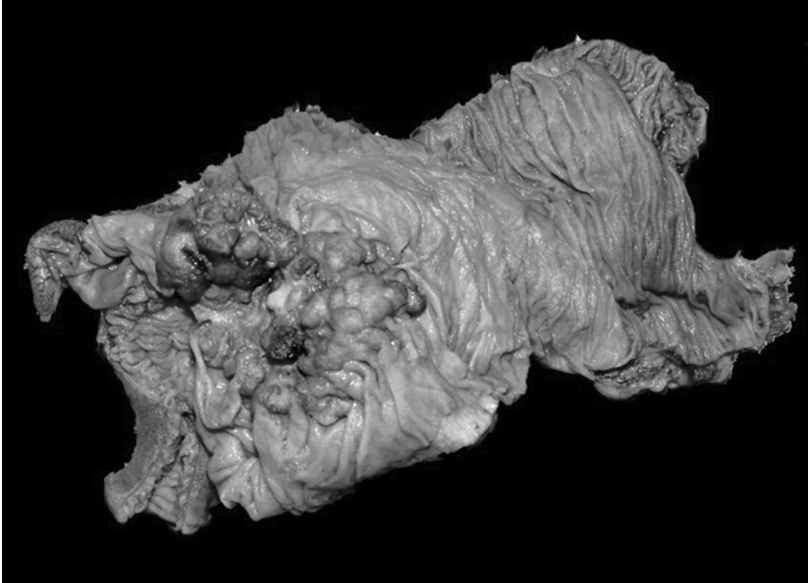
Fig1. Adenocarcinoma of the caecum. this is a right hemicolectomy specimen, in which a small piece of the terminal ileum, the caecum, the appendix, and the ascending colon have been removed. A large tumour is seen in the caecum, which was confirmed on microscopy to be an adenocarcinoma. this tumour was picked up at colonoscopy performed because the patient was found to have an unexplained iron deficiency anaemia. reproduced with permission from Clinical Pathology (Oxford Core texts), Carton, James, Daly, richard, and ramani, Pramila, Oxford University Press (2006), p.168, figure 8.20.
Molecular markers
• Current guidelines suggest that all patients with colorectal cancer should be screened for HNPCC by immunohistochemistry for loss of expression of the mismatch repair proteins MLH1, MSH2, MSH6, and PMS2. this is usually carried out on the biopsy on which the diagnosis is made.
• K-ras and BRAF mutational status is routinely requested in patients with metastatic disease and increasingly in patients with localized disease.
Prognosis
• 5- year survival rate ~50%.
• Important prognostic factors include the stage (particularly the lymph node status), presence of venous invasion, differentiation of the tumour, and completeness of surgical excision. tumour budding and the presence of extranodal lymph node deposits are additional, prognostic factors.
NHS bowel cancer screening programme
• two types of screening are offered by the NHS:
• Faecal occult blood (FOB) testing is offered every 2 y to men and women aged 60– 74. this is a home test kit sent through the post that looks for evidence of blood in the stool.
• Bowel scope screening has been, more recently, introduced in England as a one- off test to men and women at age 55. this involves direct sigmoidoscopy to look for polyps.



|
|
|
|
دراسة: الفطر سلاح فعال ضد الإنفلونزا
|
|
|
|
|
|
|
حدث فلكي نادر.. عطارد ينضم للكواكب المرئية بالعين المجردة
|
|
|
|
|
|
|
خلال شهر رمضان.. العتبة العباسية المقدسة تستعد لإقامة أنشطة دينية وثقافية في باكستان
|
|
|