

النبات

مواضيع عامة في علم النبات

الجذور - السيقان - الأوراق

النباتات الوعائية واللاوعائية

البذور (مغطاة البذور - عاريات البذور)

الطحالب

النباتات الطبية


الحيوان

مواضيع عامة في علم الحيوان

علم التشريح

التنوع الإحيائي

البايلوجيا الخلوية


الأحياء المجهرية

البكتيريا

الفطريات

الطفيليات

الفايروسات


علم الأمراض

الاورام

الامراض الوراثية

الامراض المناعية

الامراض المدارية

اضطرابات الدورة الدموية

مواضيع عامة في علم الامراض

الحشرات


التقانة الإحيائية

مواضيع عامة في التقانة الإحيائية


التقنية الحيوية المكروبية

التقنية الحيوية والميكروبات

الفعاليات الحيوية

وراثة الاحياء المجهرية

تصنيف الاحياء المجهرية

الاحياء المجهرية في الطبيعة

أيض الاجهاد

التقنية الحيوية والبيئة

التقنية الحيوية والطب

التقنية الحيوية والزراعة

التقنية الحيوية والصناعة

التقنية الحيوية والطاقة

البحار والطحالب الصغيرة

عزل البروتين

هندسة الجينات


التقنية الحياتية النانوية

مفاهيم التقنية الحيوية النانوية

التراكيب النانوية والمجاهر المستخدمة في رؤيتها

تصنيع وتخليق المواد النانوية

تطبيقات التقنية النانوية والحيوية النانوية

الرقائق والمتحسسات الحيوية

المصفوفات المجهرية وحاسوب الدنا

اللقاحات

البيئة والتلوث


علم الأجنة

اعضاء التكاثر وتشكل الاعراس

الاخصاب

التشطر

العصيبة وتشكل الجسيدات

تشكل اللواحق الجنينية

تكون المعيدة وظهور الطبقات الجنينية

مقدمة لعلم الاجنة


الأحياء الجزيئي

مواضيع عامة في الاحياء الجزيئي


علم وظائف الأعضاء


الغدد

مواضيع عامة في الغدد

الغدد الصم و هرموناتها

الجسم تحت السريري

الغدة النخامية

الغدة الكظرية

الغدة التناسلية

الغدة الدرقية والجار الدرقية

الغدة البنكرياسية

الغدة الصنوبرية

مواضيع عامة في علم وظائف الاعضاء

الخلية الحيوانية

الجهاز العصبي

أعضاء الحس

الجهاز العضلي

السوائل الجسمية

الجهاز الدوري والليمف

الجهاز التنفسي

الجهاز الهضمي

الجهاز البولي


المضادات الميكروبية

مواضيع عامة في المضادات الميكروبية

مضادات البكتيريا

مضادات الفطريات

مضادات الطفيليات

مضادات الفايروسات

علم الخلية

الوراثة

الأحياء العامة

المناعة

التحليلات المرضية

الكيمياء الحيوية

مواضيع متنوعة أخرى

الانزيمات
Anaphylaxis
المؤلف:
Stuart H. Ralston , Ian D Penman, Mark W J Strachan , Richard Hobson
المصدر:
Davidsons Principles and Practice of Medicine
الجزء والصفحة:
24th Edition , p183-184
2025-02-23
772
Anaphylaxis is a potentially life-threatening, systemic allergic reaction characterised by a variable combination of circulatory collapse, bronchospasm, laryngeal stridor, angioedema and urticaria. The risk of death is increased in patients with pre-existing asthma, particularly if this is poorly controlled, and in situations where treatment with adrenaline (epinephrine) is delayed.
Presentation
Anaphylaxis occurs when an allergen binds to and cross-links membrane-bound IgE on mast cells in a susceptible individual, causing release of histamine, tryptase and other vasoactive mediators from mast cells. These mediators have a variety of effects, including vasodilatation, increased capillary permeability leading to hypotension, and broncho constriction. It can be difficult to distinguish IgE-mediated anaphylaxis clinically from non-specific degranulation of mast cells on exposure to drugs, chemicals or other triggers where IgE is not involved, previously known as anaphylactoid reactions.
Clinical assessment
The clinical features of anaphylaxis are summarised in Figure 1. Several other conditions can mimic anaphylaxis and these are listed in Box 1 .
It is important to assess the severity of the reaction, and the time between allergen exposure and onset of symptoms provides a guide. Enquiry should be made about potential triggers. If a trigger is immediately obvious, a detailed history of the previous 24 hours may be helpful. The most common triggers of anaphylaxis are foods, latex, insect venom and drugs. A history of previous local allergic responses to the offending agent is common. The route of allergen exposure may influence the principal clinical features of a reaction; for example, if an allergen is inhaled, the major symptom is frequently wheezing. Features of anaphylaxis may overlap with the direct toxic effects of drugs and venoms. Potentiating factors, such as exercise alcohol or fatigue, can lower the threshold for an anaphylactic event. It is important to identify precipitating factors so that appropriate avoidance measures may be taken in the longer term.

Fig1. Clinical manifestations of anaphylaxis. In this example, the response is to an insect sting containing venom to which the patient is allergic. This causes release of histamine and other vasoactive mediators, which lead to the characteristic features of anaphylaxis that are illustrated.

Box1. Differential diagnosis of anaphylaxis
Investigations and management
Measurement of serum mast cell tryptase concentrations is useful to confirm the diagnosis. It is important to measure tryptase in serial tests to demonstrate the temporal relationship to the triggering event. Specific IgE tests may be useful in confirming hypersensitivity and may be prefer able to skin-prick tests when investigating patients with a history of ana phylaxis. The cornerstone of management of a severe case is the early administration of adrenaline (epinephrine), which supports the cardiovascular system, reduces bronchospasm and has some disease-modifying effects. Secondary management depends upon which organs are most affected. The emergency management of anaphylaxis is summarised in Box 2. If present, angioedema of the orofacial area requires careful observation and timely intervention, possibly with endotracheal intubation. Individuals who have recovered from an anaphylactic event should be referred for specialist assessment. The aims are to identify the trig ger, educate the patient regarding avoidance and management of sub sequent episodes, and to establish whether specific treatment, such as immunotherapy, is indicated. If the trigger factor cannot be identified or avoided, recurrence is common. Patients who have previously experienced an anaphylactic event should be prescribed self-injectable adrenaline (epinephrine) and they and their families or carers should be instructed in its use (Box 3). The use of a MedicAlert (or similar) brace let will increase the likelihood of the injector being administered in an emergency. There is an important role for a specialist dietitian when a food trigger is the suspected allergen. Allergy in adolescence requires additional consideration and management, as set out in Box 4 .

Box2. Emergency management of anaphylaxis
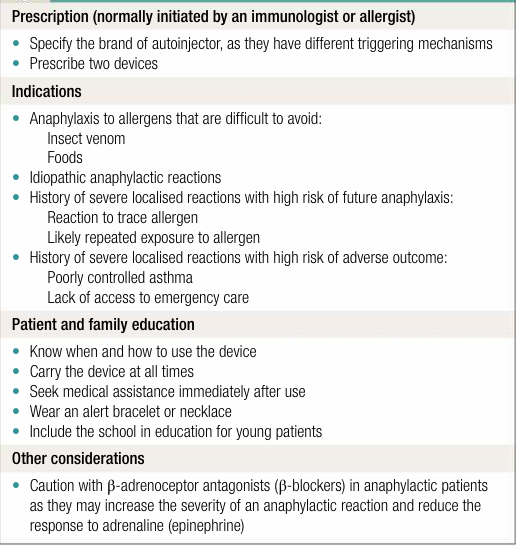
Box3. How to prescribe self-injectable adrenaline (epinephrine)

Box4. Allergy in adolescence
 الاكثر قراءة في المناعة
الاكثر قراءة في المناعة
 اخر الاخبار
اخر الاخبار
اخبار العتبة العباسية المقدسة

الآخبار الصحية















 قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة
قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة "المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة
"المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة (نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)
(نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)


















