


 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 2-1-2022
Date: 30-10-2021
Date: 23-9-2021
|
Enzymes in Clinical Diagnosis
Plasma enzymes can be classified into two major groups. First, a relatively small group of enzymes are actively secreted into the blood by certain cell types. For example, the liver secretes zymogens (inactive precursors) of the enzymes involved in blood coagulation. Second, a large number of enzyme species are released from cells during normal cell turnover. These enzymes almost always function intracellularly and have no physiologic use in the plasma. In healthy individuals, the levels of these enzymes are fairly constant and represent a steady state in which the rate of release from damaged cells into the plasma is balanced by an equal rate of removal from the plasma. Increased plasma levels of these enzymes may indicate tissue damage (Fig. 1).
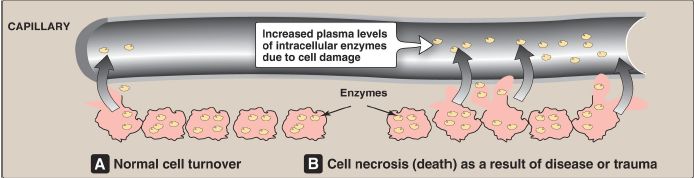
Figure 1: Release of enzymes from normal (A) and diseased or traumatized (B) cells.
Plasma is the fluid, noncellular part of blood. Laboratory assays of enzyme activity most often use serum, which is obtained by centrifugation of whole blood after it has been allowed to coagulate. Plasma is a physiologic fluid, whereas serum is prepared in the laboratory.
A. Plasma enzyme levels in disease states
Many diseases that cause tissue damage result in an increased release of intracellular enzymes into the plasma. The activities of many of these enzymes are routinely determined for diagnostic purposes in diseases of the heart, liver, skeletal muscle, and other tissues. The level of specific enzyme activity in the plasma frequently correlates with the extent of tissue damage.
Therefore, determining the degree of elevation of a particular enzyme activity in the plasma is often useful in evaluating the prognosis for the patient.
B. Plasma enzymes as diagnostic tools
Some enzymes show relatively high activity in only one or a few tissues. Therefore, the presence of increased levels of these enzymes in plasma reflects damage to the corresponding tissue. For example, the enzyme alanine aminotransferase (ALT) is abundant in the liver. The appearance of elevated levels of ALT in plasma signals possible damage to hepatic tissue. [Note: Measurement of ALT is part of the liver function test panel.] Increases in plasma levels of enzymes with a wide tissue distribution provide a less specific indication of the site of cellular injury and limits their diagnostic value.
C. Isoenzymes and heart disease
Isoenzymes (also called isozymes) are enzymes that catalyze the same reaction. However, they do not necessarily have the same physical properties because of genetically determined differences in amino acid sequence. For this reason, isoenzymes may contain different numbers of charged amino acids, which allows electrophoresis (the movement of charged particles in an electric field) to separate them (Fig. 2). Different organs commonly contain characteristic proportions of different isoenzymes. The pattern of isoenzymes found in the plasma may, therefore, serve as a means of identifying the site of tissue damage. For example, the plasma levels of creatine kinase (CK) are commonly determined in the diagnosis of myocardial infarction (MI). They are particularly useful when the electrocardiogram (ECG) is difficult to interpret such as when there have been previous episodes of heart disease.
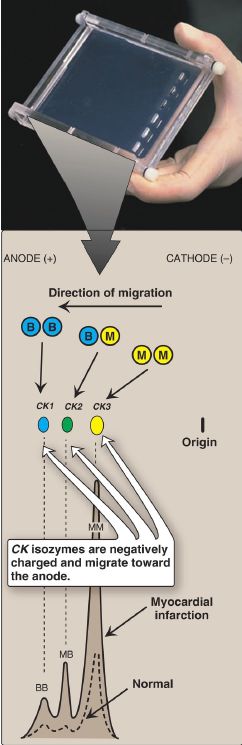
Figure 2: Subunit composition, electrophoretic mobility, and enzyme activity of creatine kinase (CK) isoenzymes.
1. Isoenzyme quaternary structure: Many isoenzymes contain different subunits in various combinations. For example, CK occurs as three isoenzymes. Each isoenzyme is a dimer composed of two polypeptides (called B and M subunits) associated in one of three combinations: CK1 = BB, CK2 = MB, and CK3 = MM. Each CK isoenzyme shows a characteristic electrophoretic mobility (see Fig. 2). [Note: Virtually all CK in the brain is the BB isoform, whereas it is MM in skeletal muscle. In cardiac muscle, about one third is MB with the rest as MM.]
2. Diagnosis of myocardial infarction: Measurement of blood levels of proteins with cardiac specificity (biomarkers) is used in the diagnosis of MI. Myocardial muscle is the only tissue that contains >5% of the total CK activity as the CK2 (MB) isoenzyme. Appearance of this hybrid isoenzyme in plasma is virtually specific for infarction of the
myocardium. Following an acute MI, CK2 appears in plasma within 4–8 hours following onset of chest pain, reaches a peak of activity at ~24 hours, and returns to baseline after 48–72 hours (Fig. 3). Troponins T (TnT) and I (TnI) are regulatory proteins involved in muscle contractility. Cardiac-specific isoforms (cTn) are released into the plasma in response to cardiac damage. They are highly sensitive and specific for damage to cardiac tissue. cTn appear in plasma within 4–6 hours after an MI, peak in 24–36 hours, and remain elevated for 3–10 days. Elevated cTn, in combination with the clinical presentation and characteristic changes in the ECG, are currently considered the “gold standard” in the diagnosis of an MI.

Figure 3: Appearance of creatine kinase isozyme CK-MB and cardiac troponin in plasma after an myocardial infarction. [Note: Either cardiac troponin T or I may be measured.]



|
|
|
|
دراسة تحدد أفضل 4 وجبات صحية.. وأخطرها
|
|
|
|
|
|
|
جامعة الكفيل تحتفي بذكرى ولادة الإمام محمد الجواد (عليه السلام)
|
|
|